The COVID-19 pandemic fundamentally changed how public health agencies approach disease surveillance, outbreak response, and population health management. What emerged from this global crisis was a clear demonstration that artificial intelligence could transform public health practice from reactive to proactive, from delayed to real-time, and from resource-intensive to efficient and scalable.
Artificial intelligence in public health encompasses computer systems performing tasks that traditionally required human intelligence to improve population health outcomes. These systems integrate machine learning, natural language processing, computer vision, and predictive analytics to process complex health datasets at unprecedented speed and scale. The growing importance of ai in public health has become undeniable as organizations worldwide recognize the potential to transform surveillance systems, outbreak response mechanisms, and health equity initiatives.
This comprehensive guide explores how ai technology is currently being deployed across public health domains, the significant benefits and persistent challenges of implementation, and the strategic frameworks needed for successful adoption. From the CDC’s innovative surveillance programs to emerging applications in precision public health, we’ll examine both the transformative potential and practical realities of integrating artificial intelligence ai into public health practice.
What is AI in Public Health and Why It Matters
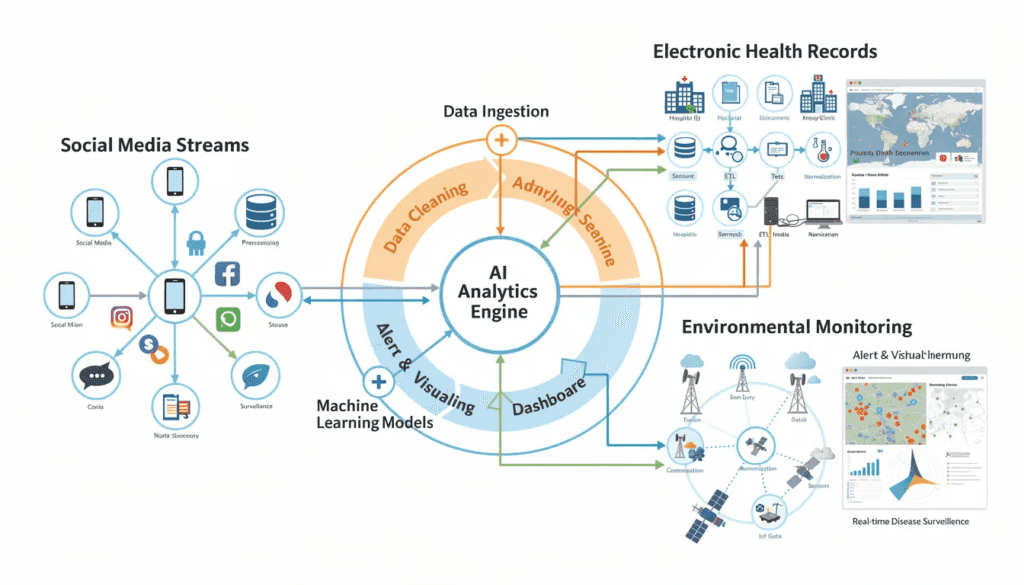
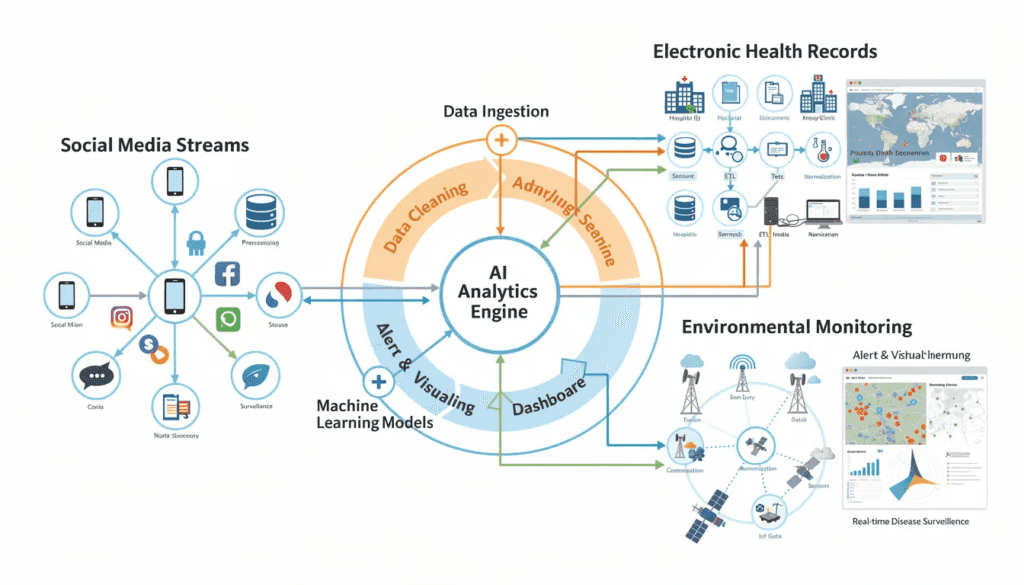
Artificial intelligence in the context of public health represents a fundamental shift from traditional manual data collection and analysis to automated, intelligent systems capable of processing vast amounts of information from electronic health records, social media platforms, environmental sensors, and genomic databases. These ai systems leverage sophisticated algorithms to identify patterns, predict outcomes, and automate decision-making processes that support public health professionals in protecting and promoting population health.

The core components of ai for public health include machine learning algorithms that learn from historical data to make predictions, natural language processing that can analyze unstructured text from health records and social media, computer vision for interpreting medical imaging and satellite data, and predictive analytics that forecast disease trends and outbreak risks. Machine learning algorithms specifically enable public health authorities to process demographic data and identify risk factors that might otherwise remain hidden in large scale data analysis efforts.
The COVID-19 pandemic served as a critical catalyst, highlighting the urgent need for rapid data analysis and real-time decision-making in public health practice. Traditional surveillance methods faced significant limitations when dealing with the speed and scale required for pandemic response. Public health agencies discovered that ai technology could accelerate response times, enhance the accuracy of outbreak detection, and support data driven decision making under extreme pressure.
The potential to transform public health surveillance extends beyond crisis response. AI models can analyze varied data sets from multiple sources simultaneously, breaking down traditional data silos that have historically limited public health effectiveness. This capability represents a significant advancement for public health departments seeking to improve health outcomes through more comprehensive and timely interventions.
The integration of ai tools with existing public health infrastructure also addresses longstanding challenges in population health monitoring. Public health organizations can now leverage artificial intelligence to identify health disparities, target interventions more effectively, and allocate resources based on predictive rather than reactive approaches. This transformation supports the broader goals of precision public health, where interventions are tailored to specific populations based on detailed analysis of multiple risk factors and demographic data.
Current AI Applications in Public Health Practice
The deployment of artificial intelligence across public health domains has accelerated rapidly, with public health agencies at federal, state, and local levels implementing ai systems for various critical functions. The CDC, world health organization, and health departments nationwide have invested significantly in ai technology, with adoption rates climbing steadily since 2020 and investment levels reaching hundreds of millions of dollars annually across the healthcare sector.
Real-world implementations demonstrate the practical value of ai in public health operations. Public health entities report substantial improvements in efficiency, accuracy, and response capabilities when ai tools are properly integrated with existing workflows. These applications span from automated data processing to sophisticated predictive modeling, each designed to support public health professionals in their essential work protecting community health.
The scope of current ai applications extends across multiple public health functions, from disease surveillance and outbreak detection to administrative efficiency and resource optimization. Public health authorities have found that machine based systems can handle routine data analysis tasks while freeing human experts to focus on strategic decision-making and community engagement activities.
Disease Surveillance and Outbreak Detection
The CDC’s National Syndromic Surveillance Program represents one of the most successful implementations of ai in public health surveillance. This system uses machine learning algorithms to analyze real-time data from emergency departments across the United States, identifying patterns that may indicate emerging public health threats or disease trends. The program processes millions of patient visits monthly, using natural language processing to extract relevant symptom information from clinical notes and electronic health records.
Real-time monitoring of social media platforms and news sources has proven particularly valuable for early outbreak signals. Research demonstrates high correlations between Twitter posts describing influenza symptoms and traditional surveillance data, enabling public health surveillance systems to detect disease trends days or weeks before conventional reporting methods. This approach leverages the fact that people often discuss health symptoms on social platforms before seeking formal medical care.
AI-powered analysis of satellite imagery provides another innovative application for environmental health threats. Machine learning models can identify environmental conditions that correlate with vector-borne disease outbreaks, such as standing water that promotes mosquito breeding or air quality changes that exacerbate respiratory conditions. These environmental monitoring capabilities enable proactive interventions before disease spread occurs.
Integration with electronic health records enables population-level disease tracking that was previously impossible at scale. AI systems can analyze de-identified patient data across multiple healthcare systems, identifying disease patterns and trends that inform public health decision making. This integration helps public health officials understand disease burden, track treatment outcomes, and identify emerging health threats across diverse populations.
The BlueDot system famously demonstrated AI’s potential by detecting COVID-19 outbreak signals in China days before official health authorities announced the outbreak. By analyzing airline ticketing data, news reports, and official health statements using natural language processing, the system identified concerning patterns and predicted the virus’s potential spread routes to other countries.
Predictive Modeling and Forecasting
The FluSight program, developed by the CDC, uses machine learning to predict influenza activity patterns across the United States. This system analyzes historical flu data, current surveillance reports, and environmental factors to forecast flu activity levels weeks in advance. The program’s predictions inform public health authorities about when and where to deploy resources for maximum impact, supporting targeted interventions and public messaging campaigns.
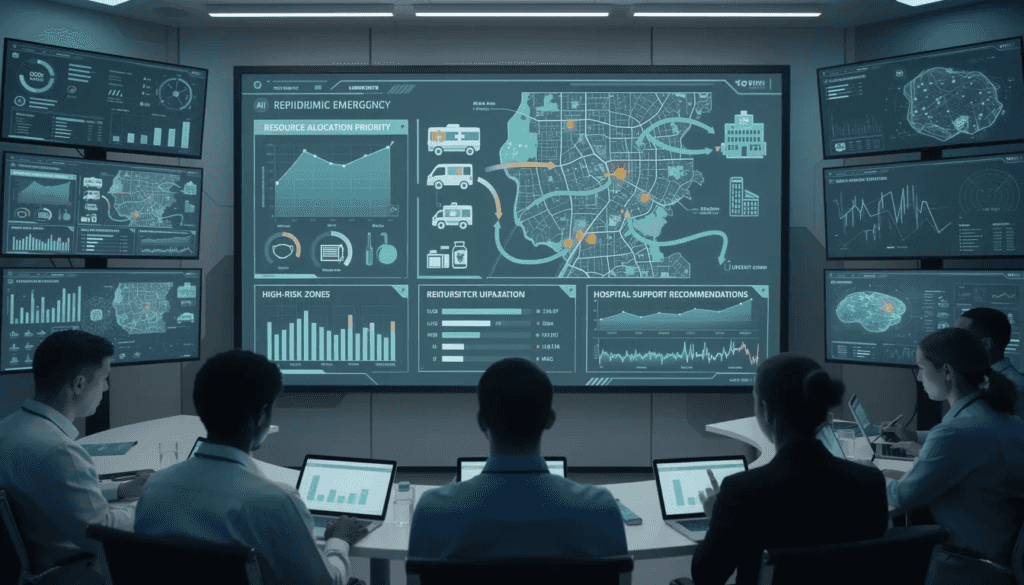
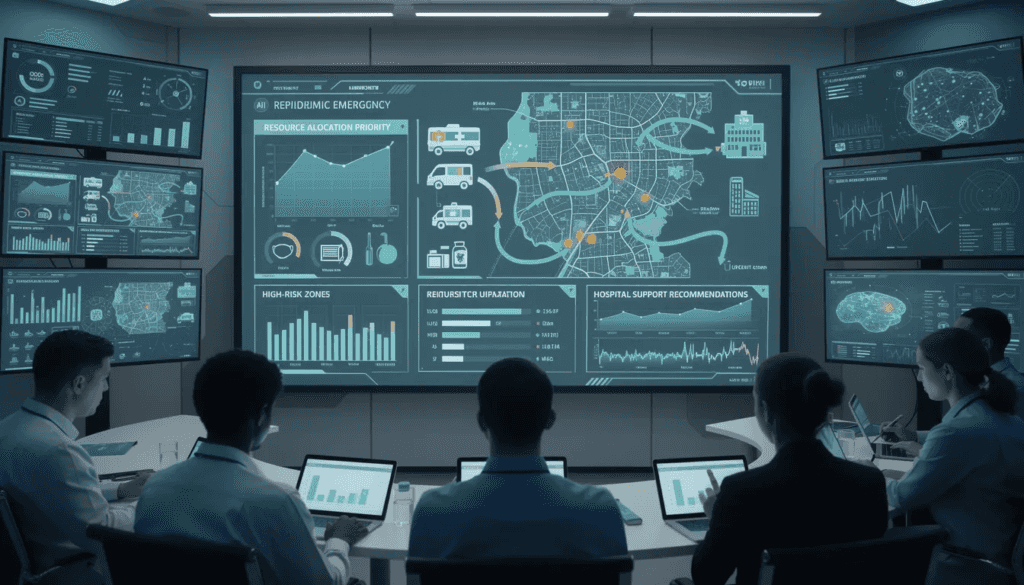
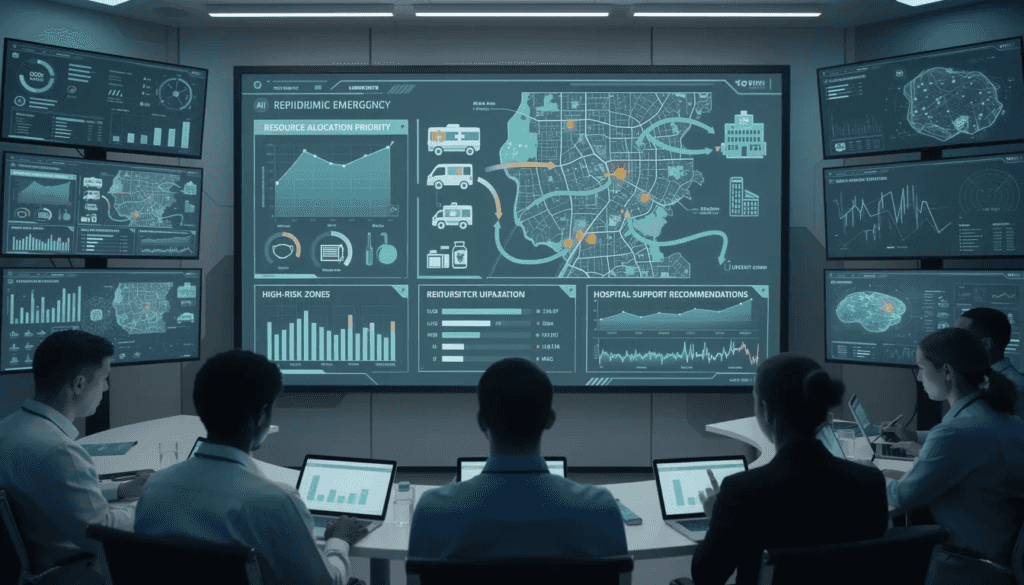
COVID-19 forecasting models became crucial tools for public health policy decisions throughout 2020-2023. These ai models processed diverse data sets including case counts, testing rates, mobility data, and vaccination coverage to predict case surges and hospitalizations. Public health officials used these predictions to guide lockdown decisions, healthcare capacity planning, and resource allocation strategies.
Climate change impact predictions represent an emerging application where ai algorithms analyze environmental data to forecast how changing weather patterns will affect vector-borne disease distribution. These models help public health departments prepare for shifting disease risks, such as expanded mosquito habitats that could increase malaria or dengue transmission in previously unaffected areas.
Population health risk stratification using ai tools enables public health authorities to identify high-risk individuals and communities for targeted interventions. Machine learning algorithms analyze demographic data, social determinants of health, and historical health outcomes to predict which populations face the greatest disease risks. This capability supports precision public health approaches that customize interventions based on specific community needs and risk factors.
Administrative Efficiency and Resource Optimization
The CDC’s implementation of ai-powered chatbots for grant report analysis demonstrates significant efficiency gains in administrative functions. This system reduced grant report analysis time by 5,500 hours annually, representing substantial cost savings and allowing staff to focus on higher-value activities. The chatbot uses natural language processing to extract key information from grant reports and identify compliance issues automatically.
Automated processing of public health data submissions and reports has streamlined workflows across multiple health departments. AI systems can validate data submissions, identify errors or inconsistencies, and route information to appropriate personnel for review. This automation reduces manual processing time and improves data quality in public health information systems.
Natural language processing applications for policy document analysis and summarization support public health authorities in staying current with rapidly evolving regulations and guidelines. These ai tools can analyze lengthy policy documents, extract key requirements, and generate summaries that help public health professionals understand compliance obligations and implementation requirements.
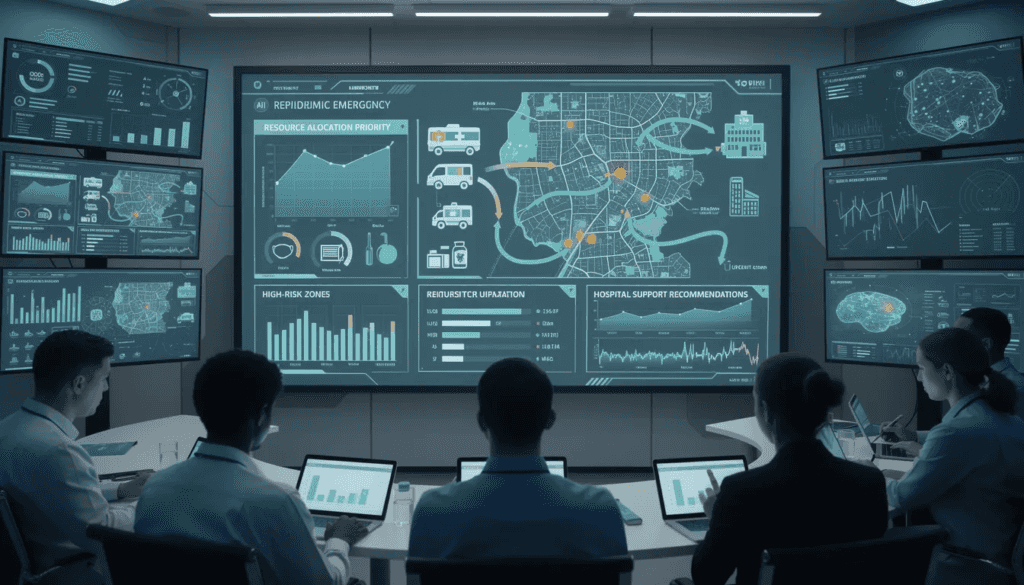
Resource allocation optimization during emergency responses has proven particularly valuable during recent public health crises. AI algorithms analyze real-time data about disease spread, healthcare capacity, and resource availability to recommend optimal distribution of personnel, equipment, and supplies. These recommendations help public health agencies maximize their impact while operating under resource constraints.
Benefits and Opportunities of AI in Public Health
The integration of artificial intelligence in public health operations delivers measurable improvements across multiple dimensions of public health practice. Enhanced speed and accuracy of public health decision making represents perhaps the most significant benefit, with ai systems capable of processing complex data sets and generating insights within hours rather than days or weeks required by traditional analytical methods.
The ability to process vast amounts of data from multiple sources simultaneously addresses a longstanding challenge in public health practice. Traditional surveillance systems often operate in isolation, limiting the comprehensive view needed for effective population health management. AI technology enables the integration of health data from electronic health records, environmental monitoring systems, social media platforms, and genomic databases to create a holistic understanding of population health status and trends.
Cost savings through automation have proven substantial across implementing organizations. The CDC reports savings of $500,000 annually through ai-powered automation of routine administrative tasks. These savings result from reduced manual labor requirements, improved accuracy that minimizes costly errors, and enhanced efficiency in data processing and analysis workflows.
Improved health equity represents a critical opportunity where ai tools can identify and address health disparities more effectively than traditional approaches. Machine learning algorithms can analyze demographic data and social determinants of health to identify populations at elevated risk for specific health conditions. This capability enables public health authorities to design targeted interventions that address root causes of health inequities.
The 24/7 monitoring capabilities provided by ai systems enable continuous surveillance that was previously impossible with human resources alone. Automated monitoring systems can detect anomalous patterns in real or virtual environments, alerting public health professionals to potential threats outside normal business hours. This continuous monitoring capability is particularly valuable for emerging infectious disease detection and environmental health threats.
Support for evidence-based policy development through real-time data analysis enables public health authorities to make decisions based on current conditions rather than outdated information. AI systems can process incoming data streams continuously, updating risk assessments and policy recommendations as new information becomes available. This capability proved crucial during the COVID-19 pandemic when conditions changed rapidly and policy decisions required frequent updates.
The scalability of ai solutions enables small health departments to access analytical capabilities previously available only to large organizations with extensive technical resources. Cloud-based ai services and pre-trained models allow health departments with limited budgets to implement sophisticated surveillance and prediction capabilities without significant upfront investments in infrastructure or technical expertise.
Implementation Challenges and Barriers
While the potential benefits of ai in public health are substantial, organizations face significant obstacles that prevent widespread adoption. Understanding these challenges is essential for developing realistic implementation strategies that balance ambitious goals with practical limitations. Public health authorities must navigate technical, workforce, and ethical challenges while maintaining focus on their core mission of protecting population health.
The complexity of implementing artificial intelligence in established public health organizations requires careful consideration of both technical requirements and organizational change management. Many health departments operate with legacy systems and processes that were designed before the digital age, creating substantial integration challenges when introducing ai technology.
Technical and Infrastructure Challenges
Limited digital infrastructure represents a primary barrier for many state and local health departments seeking to implement ai solutions. Many public health entities operate with outdated computer systems, inadequate internet connectivity, and insufficient data storage capabilities required to support machine learning algorithms and large scale data analysis. This infrastructure gap particularly affects smaller health departments that lack the resources for significant technology investments.
Data quality and standardization issues across different systems create substantial obstacles for ai implementation. Public health surveillance relies on data from multiple sources, including healthcare providers, laboratories, and community organizations, each using different data formats and standards. AI systems require high quality data with consistent formatting to function effectively, yet many public health datasets contain errors, missing values, and incompatible formats that limit their utility for machine learning applications.
Integration challenges with existing public health information systems compound these difficulties. Health departments have invested heavily in specialized software systems for specific functions such as case management, laboratory reporting, and vital statistics. Integrating ai tools with these existing systems often requires custom development work and may disrupt established workflows that public health professionals depend upon for daily operations.
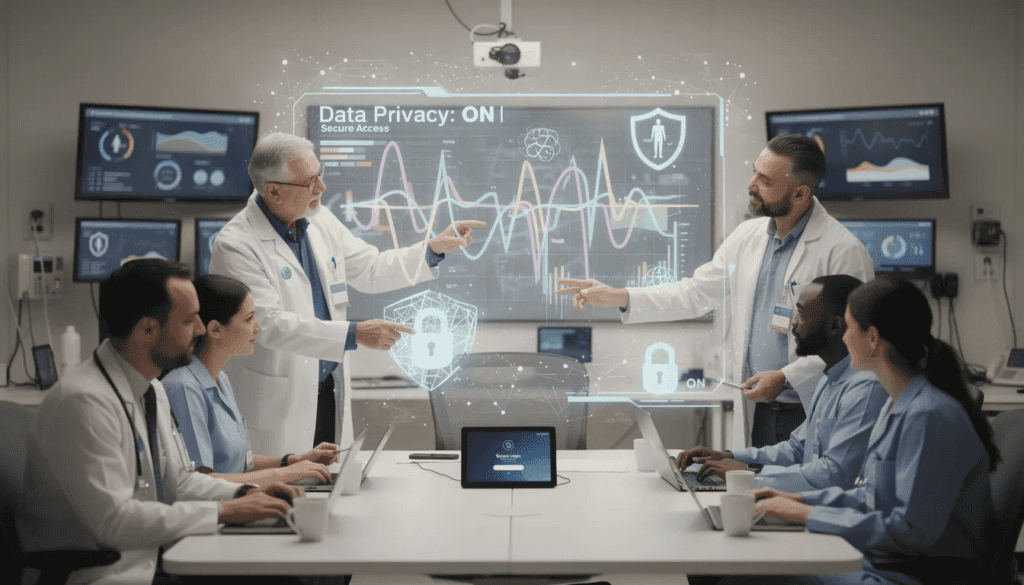
Cybersecurity concerns and data protection requirements create additional technical hurdles for ai implementation. Public health data includes sensitive information about individuals and communities that requires protection under various privacy regulations, including the general data protection regulation in international contexts. AI systems must incorporate robust security measures while maintaining the data accessibility needed for effective analysis, creating technical complexity that many health departments struggle to manage.
Workforce and Capacity Issues
The skills gap in AI and machine learning expertise among public health professionals represents a critical barrier to widespread adoption. Most public health professionals received training before ai tools became prevalent in healthcare applications, leaving them unprepared to effectively utilize these technologies. Public health organizations struggle to recruit personnel with both public health knowledge and technical ai expertise, as these individuals often command higher salaries in private sector technology companies.
Training programs and curriculum updates in schools of public health lag behind the rapid advancement of ai technology. Educational institutions face challenges in developing relevant curricula when ai applications evolve rapidly and faculty often lack practical experience with these tools. This educational gap means that new public health graduates may be unprepared to work effectively with ai systems despite growing employer expectations.
Resistance to change and technology adoption in traditional public health settings presents additional workforce challenges. Many experienced public health professionals express skepticism about ai technology based on concerns about job displacement, loss of professional autonomy, or uncertainty about the reliability of ai-generated insights. Overcoming this resistance requires extensive change management efforts and demonstration of ai’s value in supporting rather than replacing human expertise.
Competition with the private sector for AI talent creates ongoing recruitment and retention challenges for public health organizations. Technology companies can offer significantly higher compensation packages for ai specialists, making it difficult for public health agencies to compete for qualified personnel. This talent shortage limits the capacity of health departments to develop and maintain sophisticated ai systems independently.
Ethical and Equity Considerations
The risk of algorithmic bias affecting vulnerable populations disproportionately represents a serious ethical concern for ai in public health applications. Machine learning algorithms learn from historical data that may reflect existing health disparities and systemic inequities. When these biased patterns are encoded in ai systems, they can perpetuate or amplify discrimination against marginalized communities, potentially worsening health inequities rather than improving them.
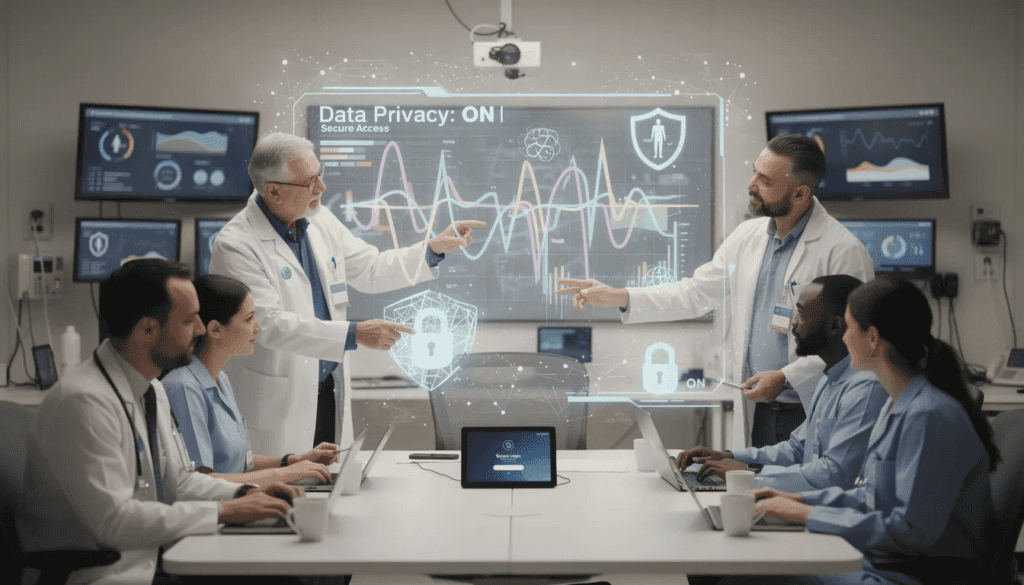
Privacy concerns with increased data collection and analysis raise significant ethical questions about the appropriate balance between population health benefits and individual privacy rights. AI systems often require access to detailed personal health information, location data, and behavioral patterns to function effectively. Public health authorities must navigate complex privacy regulations while maintaining public trust in their data practices.
Transparency and explainability requirements for AI-driven public health decisions create additional ethical challenges. Many ai algorithms operate as “black boxes” that provide predictions without clear explanations of how those predictions were generated. This lack of transparency can undermine public trust and make it difficult for public health officials to justify policy decisions based on ai recommendations.
The need for community engagement and public trust in ai systems requires ongoing effort to educate communities about how ai technology is used in public health applications. Many community members lack understanding of ai capabilities and limitations, leading to either unrealistic expectations or unnecessary fears about ai implementation. Building and maintaining public trust requires transparent communication about ai use and meaningful community involvement in decision-making processes.
Policy and Regulatory Framework
The regulatory landscape for ai in public health continues to evolve rapidly, with federal agencies, international organizations, and state governments developing frameworks to ensure responsible implementation while promoting innovation. Current federal guidance includes comprehensive White House AI initiatives that establish principles for federal agency ai use, and Office of Management and Budget (OMB) memoranda that provide specific implementation requirements for government ai systems.
The HHS AI Use Case Inventory requirements mandate that Health and Human Services agencies, including the CDC, maintain detailed records of their ai implementations, including information about system capabilities, data sources, and risk mitigation measures. These compliance measures ensure accountability and enable systematic evaluation of ai effectiveness across different public health applications.
World health organization guidelines on AI ethics in health applications provide international standards that influence policy development worldwide. These guidelines emphasize principles of transparency, accountability, and equity that inform how public health organizations implement ai technology. The WHO framework particularly emphasizes the need to address health disparities and ensure that ai benefits all populations rather than exacerbating existing inequities.
State and local policy development for responsible AI use varies significantly across jurisdictions, with some states developing comprehensive ai governance frameworks while others rely primarily on federal guidance. This policy variation creates challenges for multi-jurisdictional public health responses where consistent ai implementation across different areas would be beneficial.
International collaboration frameworks for AI in global health recognize that disease threats cross borders and require coordinated responses. These frameworks establish protocols for sharing ai-generated insights, coordinating surveillance efforts, and ensuring that ai benefits reach low-resource settings that might otherwise lack access to advanced technology.
The regulatory environment continues to evolve as policymakers balance the need to promote beneficial ai innovation while preventing potential harms. Public health organizations must stay current with changing requirements and ensure that their ai implementations comply with applicable regulations while maintaining operational effectiveness.
Building AI Capacity in Public Health Organizations

Strategic planning for health departments implementing ai requires comprehensive assessment of organizational readiness, technical requirements, and implementation priorities. Public health authorities must evaluate their current data infrastructure, workforce capabilities, and operational needs to develop realistic timelines and resource requirements for ai adoption. This planning process should identify specific use cases where ai can provide the greatest benefit while addressing existing organizational challenges.
Partnership models with academic institutions and private sector organizations offer valuable approaches for building ai capacity without requiring extensive internal technical expertise. Universities can provide research capabilities, student workforce, and technical knowledge transfer, while private companies can offer specialized ai tools and implementation support. These partnerships enable health departments to access ai capabilities while focusing their resources on public health expertise rather than technology development.
Workforce development strategies and training programs represent critical investments for successful ai implementation. Public health organizations must provide their staff with education about ai capabilities, limitations, and appropriate use cases. Training programs should emphasize how ai tools can augment human expertise rather than replace professional judgment, helping staff understand their evolving roles in ai-enhanced public health practice.
Data governance frameworks ensuring privacy and security require careful attention to both technical safeguards and policy procedures. Organizations must establish clear protocols for data access, use, and protection that comply with applicable privacy regulations while enabling effective ai implementation. These frameworks should address data quality standards, security requirements, and protocols for sharing data with external partners.
Quality assurance and continuous monitoring protocols ensure that ai systems continue to perform effectively over time. Machine learning algorithms can experience performance degradation as conditions change, requiring ongoing monitoring and recalibration. Public health organizations must establish procedures for evaluating ai system performance, identifying potential problems, and implementing corrective measures when needed.
CDC’s AI Innovation Approach
The CDC’s AI Accelerator (AIX) program demonstrates a systematic approach to scaling enterprise-wide ai solutions across a large public health organization. This program focuses on identifying high-impact use cases, developing reusable ai tools, and supporting widespread adoption across different CDC programs and offices. The AIX program prioritizes solutions that can be adapted for use across multiple public health contexts rather than developing single-purpose applications.
The AI Community of Practice connects more than 2,200 members across the CDC, providing a platform for sharing knowledge, discussing challenges, and coordinating ai development efforts. This community approach enables individual programs to benefit from lessons learned by colleagues while avoiding duplication of effort in ai development projects.
Investment in partnerships with industry, academia, and other government agencies leverages external expertise while building internal capacity. These partnerships provide access to cutting-edge ai research, specialized technical capabilities, and implementation experience that would be difficult for the CDC to develop independently.
Integration with the CDC’s Public Health Data Strategy for enhanced data sharing represents a strategic approach to maximizing the value of ai investments. By improving data quality, standardization, and accessibility across CDC systems, this integration enables more effective ai applications while supporting broader organizational goals for evidence-based decision making.
Future Directions and Emerging Trends
Generative ai applications for public health communication and education represent an emerging trend with significant potential for improving health messaging and community engagement. Large language models can generate personalized health communications, translate materials into multiple languages, and adapt messaging for different cultural contexts and literacy levels. These capabilities could significantly improve the reach and effectiveness of public health education campaigns.
Multi-modal ai systems integrating diverse data types including genomics, environmental monitoring, and social determinants of health offer unprecedented opportunities for comprehensive population health analysis. These systems can analyze patterns across multiple data domains simultaneously, identifying relationships that might not be apparent when examining individual data sources separately. This holistic approach supports precision public health initiatives that target interventions based on complex multi-factor risk profiles.
Federated learning approaches provide innovative solutions for protecting privacy while enabling collaboration across multiple organizations. This technology allows ai models to learn from distributed datasets without requiring centralized data sharing, addressing privacy concerns that often limit public health data collaboration. Federated learning could enable public health authorities to benefit from ai models trained on much larger datasets than any single organization could assemble independently.
AI-powered health equity initiatives targeting disparities represent a critical application area for future development. Advanced ai systems could identify subtle patterns of discrimination in healthcare delivery, predict which communities face the greatest health risks, and recommend specific interventions to address health disparities. These applications require careful attention to algorithmic bias prevention while leveraging ai’s pattern recognition capabilities to advance health equity goals.
Integration with Internet of Things (IoT) devices for real-time health monitoring expands the data available for ai analysis while enabling more responsive public health interventions. Environmental sensors, wearable devices, and smart city infrastructure can provide continuous data streams that ai systems analyze for early warning signs of health threats or environmental hazards.
Expected developments in ai regulation and governance through 2025-2030 will likely establish clearer standards for ai use in public health applications while potentially creating new compliance requirements. Public health organizations should anticipate more detailed regulatory frameworks and prepare for evolving requirements around ai transparency, accountability, and equity.
The evolution toward more sophisticated ai systems capable of supporting complex public health decision making represents a long-term trend that will likely transform public health practice fundamentally. These systems may eventually provide comprehensive decision support that integrates multiple data sources, considers complex trade-offs, and recommends optimal interventions for specific population health challenges.
Best Practices for Responsible AI Implementation
Human-in-the-loop approaches ensuring ai augments rather than replaces human judgment represent a fundamental principle for responsible ai implementation in public health. These approaches maintain human oversight of ai-generated recommendations while leveraging artificial intelligence to process data and identify patterns that might otherwise be missed. Public health professionals retain ultimate responsibility for decisions while benefiting from enhanced analytical capabilities.
Continuous bias monitoring and algorithm auditing processes require systematic evaluation of ai system performance across different population groups and use cases. These processes should identify potential disparities in ai system accuracy or recommendations that could disadvantage certain communities. Regular auditing enables organizations to detect and correct bias before it significantly impacts public health outcomes.
Stakeholder engagement strategies for building community trust involve transparent communication about ai capabilities, limitations, and use cases. Public health organizations should engage with community leaders, advocacy groups, and affected populations to understand concerns and incorporate feedback into ai implementation plans. This engagement builds public trust while ensuring that ai systems serve community needs effectively.
Transparent reporting of ai system capabilities and limitations helps establish realistic expectations while maintaining credibility with stakeholders. Public health organizations should clearly communicate what their ai systems can and cannot do, including information about accuracy levels, data sources, and potential sources of error. This transparency enables more effective use of ai-generated insights while preventing over-reliance on automated systems.
Regular evaluation of ai impact on health outcomes and equity ensures that ai implementations achieve their intended goals while avoiding unintended consequences. These evaluations should assess whether ai systems improve public health outcomes, reduce health disparities, and enhance organizational effectiveness. Systematic evaluation enables continuous improvement and course correction when needed.
Cross-sector collaboration models for sustainable ai development leverage expertise from multiple domains while sharing costs and risks across participating organizations. These collaborations can accelerate ai development while ensuring that solutions meet diverse needs and operate effectively in different contexts. Collaborative approaches also enable smaller organizations to access ai capabilities that would be prohibitively expensive to develop independently.
The implementation of responsible ai in public health requires ongoing commitment to ethical principles, community engagement, and continuous improvement. Organizations must balance the significant potential benefits of ai technology with careful attention to equity, privacy, and transparency concerns. Success requires both technical expertise and strong commitment to the values and mission of public health practice.
As artificial intelligence continues to evolve and mature, its role in public health will likely expand significantly. The organizations that begin implementing ai responsibly today, with careful attention to both opportunities and challenges, will be best positioned to leverage these powerful tools for protecting and promoting population health. The future of public health increasingly depends on our ability to harness artificial intelligence effectively while maintaining the human-centered values that define public health practice.
The transformation of public health through artificial intelligence represents both an unprecedented opportunity and a significant responsibility. By approaching ai implementation strategically, ethically, and collaboratively, public health organizations can realize the tremendous potential of these technologies to improve health outcomes, reduce disparities, and build more resilient communities. The time for action is now, but the approach must be thoughtful, evidence-based, and firmly grounded in public health values and objectives.